Stroke Awareness and Prevention
By Richard Fowler, MD, internal medicine physician

Contents:
According to the Centers for Disease Control and Prevention (CDC), nearly 800,000 people in the United States annually have a stroke, and the majority of these are first-time occurrences. Additional striking statistics from the CDC include:
- Every 40 seconds someone has a stroke.
- Every four minutes a person dies of a stroke.
- One in every six deaths from cardiovascular disease is due to a stroke.
- One in every four people who experience a stroke have had a stroke in the past.
- Stroke is the leading cause of disability.
- Stroke reduces mobility in >50 percent of stroke survivors ages 65 and older.
Did you know May is National Stroke Month?
Strokes can occur at any age; in fact, according to the CDC, 34% of people hospitalized in one year due to stroke were under the age of 65. So, it’s important for all of us to be aware of how to prevent strokes.
Causes of Stroke
Leading causes of stroke include:
- Advancing age
- Diabetes
- High blood pressure
- High cholesterol
- Obesity
- Prior stroke/transient ischemic attack (TIA)
- Smoking
According to the American Heart Association, one in three Americans has one of these conditions or habits.
Signs and Symptoms of Stroke
Early action is important to surviving a stroke and decreasing the long-term impacts. According to the CDC, patients who arrive at the emergency room within three hours of their first symptoms often have less disability three months after a stroke than those who received delayed care.
Unfortunately, many people do not recognize all the signs and symptoms of a stroke. In fact, the CDC reports that in one survey, only 38 percent of respondents were aware of all major symptoms and knew to call 9-1-1 when someone was having a stroke.
While most people recognize sudden numbness on one side as a sign of a stroke, below are other signs and symptoms of a stroke. Note that all these signs or symptoms occur suddenly.
- Confusion, trouble speaking, or difficulty understanding speech
- Dizziness, lack of coordination, loss of balance or trouble walking
- Severe headache with no known cause
- Trouble seeing in one or both eyes
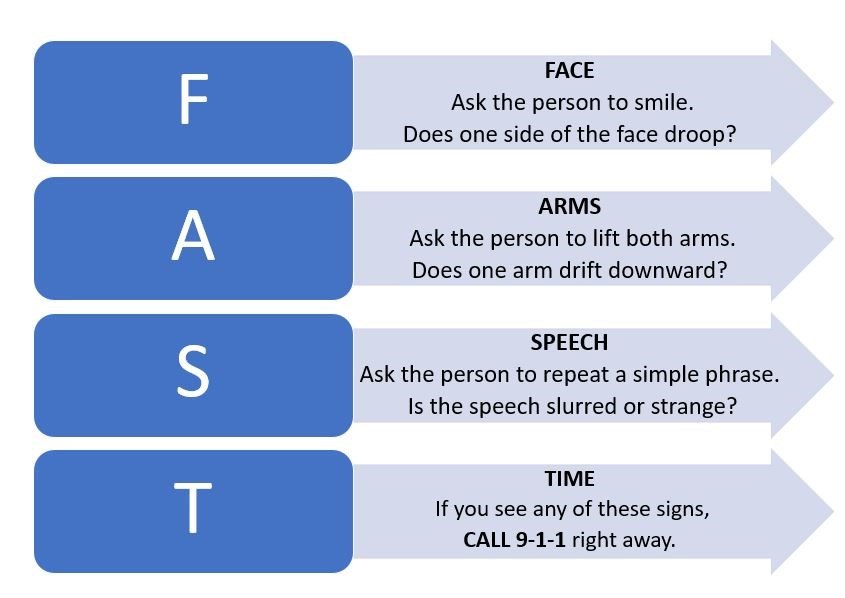
F.A.S.T. to Save Lives
If you recognize signs or symptoms of a stroke in someone, follow these steps:

















 Anyone who knows Dr. Filner knows that when he is not caring for patients, he can be found riding his Harley. In Arizona, we are fortunate to have many great months for long rides due to Arizona having more sunny days (85-90 percent per year) than almost all other states. In fact, we have more sunny days per year than California and Florida.
Anyone who knows Dr. Filner knows that when he is not caring for patients, he can be found riding his Harley. In Arizona, we are fortunate to have many great months for long rides due to Arizona having more sunny days (85-90 percent per year) than almost all other states. In fact, we have more sunny days per year than California and Florida.